By Dr Sanjay Kumar, Department of Cardiothoracic and Vascular Surgery (CTVS) at Medanta Super Speciality Hospital, Noida

Heart valve replacement is a surgical procedure used when a damaged heart valve cannot be repaired. In this surgery, the diseased valve is replaced with a biological (tissue) valve or a mechanical valve. Biological valves usually last 10 to 20 years, while mechanical valves can last a lifetime but require long-term blood-thinning medication to prevent clots. Valve replacement is a widely used and effective treatment for conditions such as aortic valve disease and mitral valve disease.
What Is Heart Valve Replacement?
Heart valve replacement is a surgical or minimally invasive procedure used to replace a damaged heart valve with a new one. The new valve can be biological, made from animal or human tissue, or mechanical, made from durable artificial materials.
This procedure is recommended for people with severe heart valve disease, especially when the heart is unable to pump blood effectively or when symptoms such as chest pain, breathlessness, dizziness, or fainting occur.
The heart has four valves—aortic, mitral, tricuspid, and pulmonary. While surgeons can replace any of these valves, the aortic valve is most commonly replaced, followed by the mitral valve. Replacement of the tricuspid and pulmonary valves is less common.
Heart valve replacement is an effective treatment for:
- Aortic valve disease
- Mitral valve disease
- Tricuspid valve disease
- Pulmonary valve disease
- Congenital heart disease
Types of Replacement Heart Valves
A replacement heart valve is known as a prosthetic or artificial valve. There are two main types of replacement valves used in heart valve surgery.
1. Biological (Tissue) Valves
Biological valves, also called tissue or bioprosthetic valves, are made from animal or human tissue. These may include tissue from cows (bovine), pigs (porcine), or donated human valves (homografts). Some biological valves may also contain small artificial components.
Advantages:
- Usually do not require lifelong blood-thinning medication
- No clicking sound after surgery
Limitations:
- Less durable than mechanical valves
- Typically lasts 10 to 20 years
- May require another valve replacement surgery in the future
2. Mechanical Valves
Mechanical valves are made from strong materials such as metal or carbon. The most common type is the bileaflet valve, which consists of two carbon flaps mounted in a fabric-covered ring. These valves are extremely durable and well-tolerated by the body.
Advantages:
- Very long-lasting and may last a lifetime
Limitations:
- Require lifelong blood-thinning medication (such as warfarin) to prevent clot formation
- Regular blood tests are needed to monitor medication levels
- Some patients may hear a soft clicking sound from the valve opening and closing
How the Right Valve Is Chosen
The choice between a biological and mechanical valve is made carefully and jointly between the patient and the surgeon.
The Director, Cardiovascular & Thoracic Surgery (Medanta Super Speciality Hospital, Noida) considers several important factors, including:
- Your age
- Risks associated with long-term blood thinner use
- The possibility of needing another surgery later in life
- Your lifestyle and personal preferences
This shared decision-making approach ensures that the selected valve best suits your health needs and long-term well-being.
Procedure Details
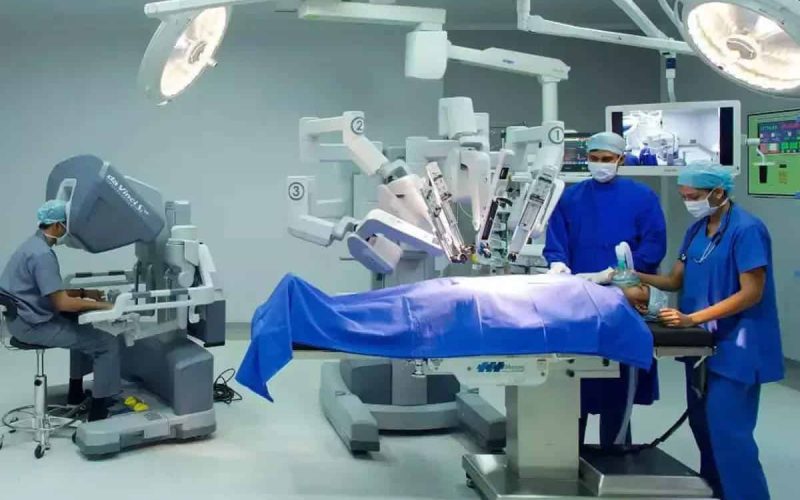
Which Surgery Is Best for Heart Valve Replacement?
Heart valve replacement can be done using traditional open-heart surgery or minimally invasive catheter-based procedures. The best option depends on several factors, including the type of valve disease, your age, overall health, surgical risk, the structure of the valve, and your heart function.
Traditional (Open-Heart) Valve Surgeries
These procedures involve opening the chest to replace the damaged valve and may include:
- Surgical Aortic Valve Replacement (SAVR)
- Ross Procedure
- Mitral Valve Replacement Surgery
- Tricuspid Valve Replacement Surgery
Catheter-Based (Minimally Invasive) Valve Procedures
These procedures use small cuts and thin tubes (catheters) and are becoming increasingly common, especially for aortic valve disease. They include:
- TAVR ( Transcatheter Aortic Valve Replacement )
- Transcatheter Mitral Valve Replacement (TMVR)
- Transcatheter Pulmonary Valve Replacement (TPVR)
Your surgeon will carefully explain which option is most suitable for you, along with the expected benefits, possible risks, recovery time, and follow-up care.
How Should I Prepare for Heart Valve Replacement?
Before the procedure, you will receive detailed preparation instructions, which may include:
- When to stop eating or drinking
- Which regular medicines should be stopped or continued?
- Blood tests, imaging, or other tests a day before surgery
Wear comfortable clothing and shoes that are easy to put on. You will also need someone to accompany you and drive you to and from the hospital.
What Happens During Heart Valve Replacement?
The exact steps depend on whether you are having open-heart surgery or a catheter-based procedure. In general, the process includes:
- Preparing the incision site
The area is cleaned and shaved to minimise the risk of infection. - Anesthesia
You are given anaesthesia so you sleep during the procedure and feel no pain. - Making the incision
The incision may be in the centre of the chest, between the ribs, or in the groin, depending on the procedure. - Heart-lung machine (if needed)
For open-heart surgery, a heart-lung machine temporarily takes over heart and lung function. This is not required for catheter-based procedures. - Valve replacement
The diseased valve is removed and replaced with a biological or mechanical valve. In some catheter-based procedures, the new valve is placed inside the existing valve. - Closing the incision and recovery
Once the new valve is confirmed to be working properly, the incision is closed, and you are moved to the recovery area.
Heart valve replacement procedures usually take 1 to 4 hours. Catheter-based procedures are generally shorter than open-heart surgeries.
Benefits and Risks of Heart Valve Replacement
Benefits
Heart valve replacement:
- Treats the root cause of valve disease
- Relieves symptoms such as breathlessness and chest pain
- Improves quality of life
- Helps patients live longer
Catheter-based procedures often offer:
- Shorter hospital stays
- Faster recovery
- Lower risk of infection
However, open surgery may be the better option in certain complex cases.
Potential Risks
As with any major heart procedure, risks may include:
- Infection
- Bleeding
- Abnormal heart rhythm
- Heart attack
- Heart or kidney failure
Your healthcare provider will explain the specific benefits and risks based on your condition and the chosen procedure.
Recovery and Outlook
What Happens After Heart Valve Replacement?
After your heart valve replacement, you will begin recovery in the intensive care unit (ICU), where your medical team will closely monitor your heart, breathing, and overall condition. Once you are stable, you will be shifted to a regular hospital room.
Your care team will inform you how long you need to stay in the hospital. Many patients are also advised to take part in cardiac rehabilitation, a supervised program that helps them regain strength, improve heart health, and recover safely after valve replacement.
What Is the Recovery Time?
For most people, recovery after heart valve replacement takes about one to three months. Recovery is usually faster with minimally invasive or catheter-based procedures than with open-heart surgery.
During recovery, you can generally expect:
- Feeling tired or weak for the first few weeks
- Temporary restrictions on driving
- Limits on physical activities, such as lifting heavy objects
- A gradual return to work after several weeks or months
Your healthcare provider will guide you on what activities are safe and when you can slowly return to your normal routine.
Is Heart Valve Replacement Major Surgery?
Yes, heart valve replacement is considered major heart surgery. It is natural to worry about how it may affect your daily life and recovery time. Patients who undergo less invasive procedures often recover more quickly than those who have open-heart surgery. However, recovery varies from person to person.
Your provider will explain what to expect based on your specific procedure and overall health.
When Should I Call My Healthcare Provider?
Contact your healthcare provider during recovery if you experience:
- Fever or chills
- An irregular or fast heartbeat
- Pain, redness, swelling, bruising, or discharge at the incision site
- Pain, swelling, or discolouration in your lower leg (possible sign of a blood clot)
- Sudden weight gain or swelling in your legs or feet
If you are taking blood-thinning medication, inform your provider if you fall—even if you feel fine—or if you notice unusual bleeding, such as from your gums or nose.
Seek emergency medical care immediately if you have symptoms of a heart attack or stroke.
A Reassuring Note for Patients
Receiving a new heart valve can bring many emotions—fear, relief, anxiety, or hope. These feelings are completely normal. Heart valve replacement is a common and well-established procedure, and advances in medical technology have made it safer and more successful than ever before.
Your healthcare team will support you at every step of the journey and help you feel confident about your recovery and long-term heart health.
Frequently Asked Questions
1. How long does a heart valve replacement last?
The lifespan of a replaced valve depends on the type used.
- Mechanical valves can last 20–30 years or longer but usually require lifelong blood thinners.
- Biological (tissue) valves last about 10–20 years and may not require long-term blood thinners.
2. Is heart valve replacement safe?
Yes. Heart valve replacement is a commonly performed and well-established procedure. With modern surgical techniques and minimally invasive options, success rates are high, especially when done at experienced cardiac centers.
3. Will I need to take medicines after valve replacement?
Yes. Most patients need medications after surgery, which may include blood thinners, antibiotics (before certain procedures), and heart medicines. Your doctor will decide based on the type of valve and your overall health.
4. Can I live a normal life after valve replacement?
Most patients return to a normal, active life after recovery. Many experience improved energy levels, better breathing, and relief from symptoms like chest pain or fatigue.
5. Is open-heart surgery always required?
No. Many patients can now be treated with catheter-based procedures like TAVR or TMVR, which do not require opening the chest. Your doctor will choose the best option based on your condition.
6. How painful is recovery after valve replacement?
Some discomfort is normal, especially after open-heart surgery, but pain is well-managed with medication. Minimally invasive procedures usually cause less pain and allow faster recovery.
7. When can I return to work after surgery?
Most people return to work within 6 to 12 weeks, depending on the type of procedure and the nature of their job. Your doctor will guide you based on your progress.
8. Do I need lifestyle changes after valve replacement?
Yes. A heart-healthy lifestyle is important. This includes:
- Regular exercise (as advised)
- Healthy diet
- Avoiding smoking
- Managing blood pressure, diabetes, and cholesterol
9. What are the warning signs after surgery?
Contact your doctor immediately if you notice fever, chest pain, shortness of breath, irregular heartbeat, swelling, or signs of infection at the incision site.
10. Will I need follow-up visits after valve replacement?
Yes. Regular follow-ups, heart scans (echocardiograms), and blood tests are essential to ensure your new valve is working properly.
Final Thought
Heart valve replacement is a life-saving and life-improving procedure for people with severe valve disease. While it is major surgery, advancements in medical technology have made treatment safer, recovery faster, and outcomes better than ever before. With the right procedure, proper care, and regular follow-ups, most patients go on to live active, fulfilling lives. If you have symptoms or concerns about your heart valves, early consultation with a cardiac specialist can make a significant difference in your long-term health.